Invisible illnesses
And the people who suffer from them (like me)
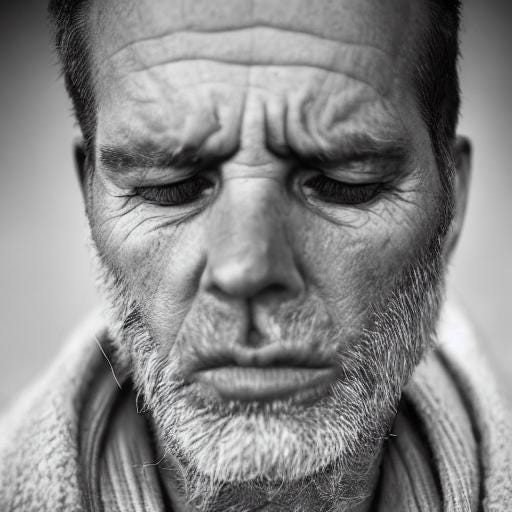
If you see me walking around, it is unlikely you will think to yourself: that person is mentally ill. Yet I am. I have severe PTSD from spending time in war zones. That PTSD most likely started earlier, before I was a marine or a soldier.
Post-traumatic stress disorder (PTSD) is a mental health condition that's triggered by witnessing or experiencing a terrifying event. It's a disorder that can change a person psychologically and physiologically.
The most profound changes occur in the brain itself. Specifically, PTSD can affect three areas: the amygdala, the hippocampus, and the prefrontal cortex. When the amygdala, responsible for fear responses, is overactive, anxiety and hypervigilance can occur. The hippocampus, which helps process memories, can shrink, causing difficulties with memory and concentration. Finally, the prefrontal cortex, which controls executive functions and decision-making, can become impaired, leading to problems with impulse control and rational thinking. In my case, undiagnosed ADHD was already impairing executive functions and decision-making. I got the double-whammy.
PTSD also triggers changes in the body's stress hormones. Long-term exposure to the stress hormone cortisol can damage neurons, compromise the immune system, and even alter the body's DNA. This can cause chronic health problems, such as heart disease, diabetes, and autoimmune disorders. In addition, PTSD can change a person's behavior, leading to sleep disturbances, avoidance of certain situations, and struggles with anger and irritability. Sometimes, despite being medicated, I scream in my sleep. Sometimes I also punch my demons. And if you happen to being sleeping next to me, watch out.
With the right treatment, such as cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), or medication, individuals can learn to manage their symptoms and improve their quality of life. Studies have even shown that the brain has an amazing ability to heal and rewire itself, a process known as neuroplasticity. It only took me a decade to ask for help, and another decade to get properly diagnosed.
Living with PTSD can also lead to profound personal growth. Many survivors report increased resilience, deeper empathy, and a greater appreciation for life. Remember, our experiences don't define us - it's what we do with them that truly matters. We are not bound by the past, but we can shape our own future. I just tattooed myself with the words, “Kindness Matters.” That’s because I want to remember that anyone I meet could have experienced horrific trauma, just as I have. Kindness is free. It costs me nothing to offer it to others.
In conclusion, while PTSD can change a person, we should not lose sight of the innate strength and potential for growth that lies within each of us. There is always a path forward, a route to recovery, and a hope for a better tomorrow. The human spirit is resilient, and with the right support and resources, individuals battling PTSD can reclaim their lives and thrive in the face of adversity.
Examples of PTSD:
Consider the story of James, a former military officer who served in conflict zones. After returning home, he battled severe PTSD symptoms, including intense nightmares and social withdrawal. With the support of a dedicated mental health care team and the utilization of cognitive-behavioral therapy, James regained a measure of control over his life. Today, he uses his experience to advocate for better mental health services for veterans and supports others dealing with similar struggles.
Or take Lisa, a survivor of a devastating natural disaster. The trauma left her with debilitating fear, unable to function in her day-to-day life. However, through EMDR therapy and mindfulness techniques, she processed her traumatic experience and manage her anxiety. Now, she works as a disaster relief volunteer, transforming her painful memories into a force for good.
These are just examples, but they highlight the potential for recovery and personal growth in the face of PTSD. It's a testament to the strength of the human spirit and the power of proper treatment and support.
According to the American Psychiatric Association, 3.5% of adults in the United States suffer from Post-Traumatic Stress Disorder (PTSD) each year. This equates to about eight million people grappling with this condition annually. In the United States, which is 5% of the world’s humans. Globally, the World Health Organization estimates that over 7% of the population will experience PTSD in their lives. These figures underline the crucial need for awareness, understanding, and effective treatment strategies around the world.
Post-traumatic stress disorder (PTSD) is a mental health condition that's triggered by witnessing or experiencing a terrifying event. It's a disorder that can fundamentally change a person psychologically and physiologically.
The most profound changes occur in the brain itself. Specifically, PTSD can affect three areas: the amygdala, the hippocampus, and the prefrontal cortex. When the amygdala, responsible for fear responses, is overactive, anxiety and hypervigilance can occur.. The hippocampus, which helps process memories, can shrink, causing difficulties with memory and concentration. Finally, the prefrontal cortex, which controls executive functions and decision-making, can be impaired, leading to problems with impulse control and rational thinking.
PTSD also triggers changes in the body's stress hormones. Long-term exposure to the stress hormone cortisol can damage neurons, compromise the immune system, and even alter the body's DNA. This can result in chronic health problems such as heart disease, diabetes, and autoimmune disorders. In addition, PTSD can change a person's behavior, leading to sleep disturbances, avoidance of certain situations, and struggles with anger and irritability.
Despite these challenges, it's important to remember that there's hope. PTSD is not a life sentence. With the right treatment, such as cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), or medication, individuals can learn to manage their symptoms and improve their quality of life. Studies have even shown that the brain has an amazing ability to heal and rewire itself, a process known as neuroplasticity.
Moreover, living with PTSD can also lead to profound personal growth. Many survivors report increased resilience, deeper empathy, and a greater appreciation for life. Remember, our experiences don't define us - it's what we do with them that truly matters. We are not bound by the past, but rather, we have the capacity to shape our own future.
In conclusion, while PTSD can change a person in many ways, we should not lose sight of the innate strength and potential for growth that lies within each of us. There is always a path forward, a route to recovery, and a hope for a better tomorrow. The human spirit is resilient, and with the right support and resources, individuals battling PTSD can reclaim their lives and thrive in the face of adversity.
Consider the story of James, a former military officer who served in conflict zones. After returning home, he battled severe PTSD symptoms, including intense nightmares and social withdrawal. With the support of a dedicated mental health care team and the utilization of cognitive-behavioral therapy, James was able to regain control over his life. Today, he uses his experience to advocate for better mental health services for veterans and supports others dealing with similar struggles.
Or take Lisa, a survivor of a devastating natural disaster. The trauma left her with debilitating fear, unable to function in her day-to-day life. However, through EMDR therapy and mindfulness techniques, she was able to process her traumatic experience and manage her anxiety. Now, she works as a disaster relief volunteer, transforming her painful memories into a force for good.
These are just examples, but they highlight the potential for recovery and personal growth in the face of PTSD. It's a testament to the strength of the human spirit and the power of proper treatment and support.
According to the American Psychiatric Association, approximately 3.5% of adults in the United States suffer from Post-Traumatic Stress Disorder (PTSD) each year. This equates to nearly 8 million people grappling with this condition annually. More globally, the World Health Organization estimates that over 7% of the population will experience PTSD at some point in their lives. These figures underline the crucial need for awareness, understanding, and effective treatment strategies around the world.
While we celebrate stories of recovery and resilience, it is vital to recognize the darker side of PTSD: the tragically high suicide rates among those battling the condition. According to the U.S. Department of Veterans Affairs, suicide rates among veterans diagnosed with PTSD are nearly twice as high as the general population. Similarly, the National Institute of Mental Health cites PTSD as a significant risk factor for suicide across all demographics. These statistics illuminate a sobering reality. But they also underscore the urgent need for comprehensive, accessible mental health services and ongoing support for those living with PTSD. Remember, treatment can save lives, and no one should have to fight this battle alone.
The Veterans Affairs (VA) has a well-defined rating system in place to diagnose and treat veterans with Post-Traumatic Stress Disorder (PTSD). This system plays a pivotal role in determining the level of disability and hence, the compensation that a veteran is entitled to receive. VA ratings for PTSD range from 0 to 100 percent, in increments of 10. A rating of 0 percent implies that while the condition is recognized, it has not impaired the veteran's ability to function socially or at work. On the opposite end of the spectrum, a 100 percent disability rating signifies total impairment, where PTSD has severely hindered the veteran's ability to function in daily life. Here, it's crucial to note that a higher rating leads to increased financial compensation to assist the veteran in managing the disorder. This rating system is a testament to the VA's commitment to acknowledging and addressing PTSD amongst veterans, thereby emphasizing the significance of mental health care in overall well-being.
A 70% rating for PTSD, as defined by the VA, indicates a high level of disability. Veterans with this rating often showcase symptoms such as chronic depression or anxiety, difficulty in understanding complex commands, and impaired judgment. They may also experience difficulty in establishing and maintaining effective relationships, suicidal ideation, and have a near-continuous state of panic or depression affecting the ability to function independently or effectively. Regardless of these significant challenges, it is essential to remember that there is hope and help available. With appropriate treatment, support, and commitment, individuals at this level can work towards managing their symptoms and improving their overall quality of life. The 70% rating also ensures a higher degree of financial support, demonstrating the VA's recognition of this critical need and their commitment to assisting veterans in their journey towards recovery.
Welcome to the dark side
It is vital to recognize the darker side of PTSD: the tragically high suicide rates among those battling the condition. According to the U.S. Department of Veterans Affairs, suicide rates among veterans diagnosed with PTSD are twice as high as the general population. Similarly, the National Institute of Mental Health cites PTSD as a significant risk factor for suicide across all demographics. These statistics illuminate a sobering reality. But they also underscore the urgent need for comprehensive, accessible mental health services and ongoing support for those living with PTSD. Remember, treatment can save lives, and no one should have to fight this battle alone.
The Veterans Affairs (VA) has a well-defined rating system in place to diagnose and treat veterans with Post-Traumatic Stress Disorder (PTSD). This system plays a pivotal role in determining the level of disability and, hence, the compensation that a veteran may receive. VA ratings for PTSD range from 0 to 100 percent, in increments of 10. A rating of 0 percent implies that, while they recognize the condition, it has not impaired the veteran's ability to function socially or at work. On the opposite end of the spectrum, a 100 percent disability rating signifies total impairment, where PTSD has severely hindered the veteran's ability to function in daily life. Here, it's crucial to note that a higher rating leads to increased financial compensation to assist the veteran in managing the disorder. This rating system is a testament to the VA's commitment to acknowledging and addressing PTSD amongst veterans, emphasizing the significance of mental health care in overall well-being.
My current rating is 70%
A 70% rating for PTSD, as defined by the VA, shows a high level of disability. Veterans with this rating often showcase symptoms such as chronic depression or anxiety, difficulty in understanding complex commands, and impaired judgment. They may also experience difficulty in establishing and maintaining effective relationships, suicidal ideation, and have a near-continuous state of panic or depression affecting the ability to function independently or effectively. Regardless of these significant challenges, it is essential to remember that there is hope and help available. With treatment, support, and commitment, individuals at this level can work towards managing their symptoms and improving their overall quality of life. The 70% rating also ensures a higher degree of financial support, demonstrating the VA's recognition of this critical need and their commitment to assisting veterans in their journey towards recovery.
If you see me walking around, or on a videoconference, or flying my drone to make a video reminding me that some of this world is beautiful, and that I still have reasons to live, please be kind. To me or someone else. There is more than enough trauma to go around - don’t add to it if you can offer something better.
If you have PTSD, and you need someone to listen, encourage, or just sit with you for a while, I will be that person if I can. On my better days, I can be a pretty good human. I’ll do my best for you. Despite, or because of, my invisible illness.
I mostly keep my suffering to myself, but I want to help you carry yours until you are ready to let go of it. If you get to that point.
Thank you for reading.




"Be kind whenever possible ~ it is always possible"
Your kind offer to support others in need is generous.
Thank you for sharing your story.